Key Takeaways
- Heavy metal toxicity can originate from environmental, dietary, and occupational sources, and recognizing early symptoms is crucial.
- Regular screening, timely diagnosis, and prompt action dramatically improve outcomes for those affected.
- Preventive habits and awareness are essential for reducing exposure and long-term risk.
- Innovative therapies are emerging to enhance the removal of heavy metals and minimize health consequences.
Understanding Heavy Metal Toxicity
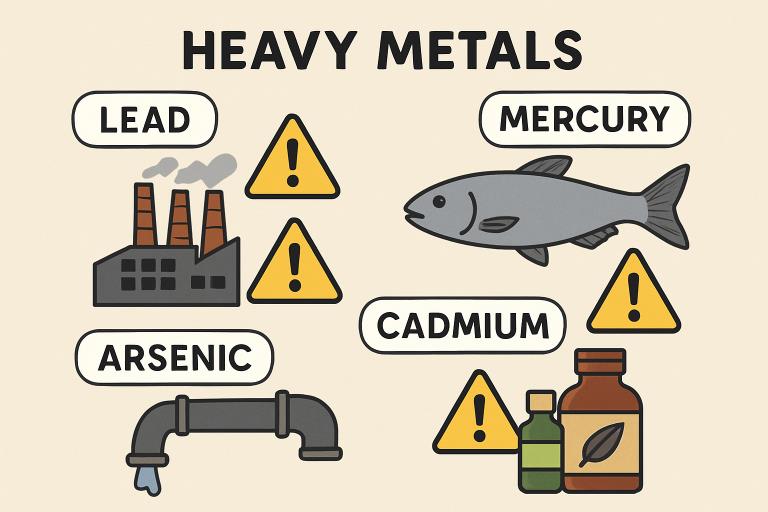
Heavy metal toxicity, a growing health concern globally, occurs when metals such as lead, mercury, arsenic, or cadmium accumulate in the human body over time and interfere with key physiological processes. These metals have no biological role and are particularly harmful because the body struggles to eliminate them efficiently. Problems can develop stealthily and go unnoticed until significant damage occurs. For anyone concerned about managing exposures or seeking support for detoxification, there are now specialized heavy metal toxicity treatment options that target the root causes and provide hope for those affected.
These metals can enter various bodily systems through food, water, air, or direct skin contact, often causing acute or chronic symptoms depending on dose and duration. Reinforcing the necessity of vigilance, both public health authorities and clinicians emphasize education, early recognition, and careful assessment of at-risk populations. Proactively understanding the pathways and risks can make all the difference in prevention and recovery.
Common Sources of Heavy Metal Exposure
- Industrial Emissions:Many factories emit pollutants, such as cadmium and mercury, which can settle in soil and water.
- Contaminated Water:Lead pipes, outdated plumbing, or proximity to mining can taint water supplies with hazardous metals.
- Seafood Consumption:Fish, especially larger species like tuna and swordfish, may bioaccumulate mercury, posing risks with frequent consumption.
- Traditional Medicines:Certain folk remedies and imported herbal products may be contaminated with heavy metals like lead or arsenic.
Urban environments with aging infrastructure and industrial activities pose heightened risks, especially in vulnerable communities. Even natural disasters can mobilize previously buried toxins, making periodic testing essential for populations in affected regions.
Symptoms Indicating Heavy Metal Poisoning
The symptoms of heavy metal poisoning can vary widely based on the metal, degree of exposure, age, and underlying health status of the individual. According to WebMD, acute exposures can lead to overt symptoms, while chronic low-level exposure often produces subtle, slowly worsening complaints that may be mistaken for other common conditions. Hallmark symptoms include:
- Abdominal pain, nausea, and gastrointestinal distress
- Memory loss, difficulty concentrating, or personality changes
- Chronic fatigue unrelieved by rest
- Declining kidney function or abnormal lab markers
- Cardiovascular complications, such as hypertension or arrhythmias
Children are particularly vulnerable, often showing developmental regression, learning delays, or behavioral changes. Neurological impacts in adults and children can persist even after exposure ends, emphasizing the need for public health vigilance.
Diagnostic Approaches for Heavy Metal Toxicity
Accurate diagnosis of heavy metal toxicity typically involves a combination of exposure history, clinical findings, and laboratory testing. Medical providers may use blood, urine, hair, or, occasionally, tissue samples to detect elevated metal levels. Patients are advised to avoid high-mercury fish and other sources of variable exposure prior to testing, as these may distort measurement results. Advanced diagnostics also play an essential role in screening occupational groups or residents in affected localities. Regular monitoring is vital for individuals in professions with known exposure risks, such as battery manufacturing, mining, or laboratory work.
Effective Treatment Strategies
Treatment of heavy metal toxicity starts with immediate actions to prevent further exposure—identifying and eliminating the primary source is critical to halting progression. Medical management then typically consists of:
- Chelation Therapy:Chelating agents, such as EDTA or DMSA, bind heavy metals and facilitate their excretion in urine. Treatment plans are customized based on the specific metal and the patient’s overall health.
- Supportive Care:Addressing dehydration, electrolyte imbalances, or organ dysfunction is essential, especially in severe cases. Long-term monitoring may be needed to track recovery and prevent relapse.
Adjunct therapies, such as nutritional support and antioxidant supplementation, may support the body’s natural detoxification processes.
Preventive Measures to Reduce Risk
Prevention is indisputably the most effective strategy for tackling heavy metal toxicity. Individuals—and parents, in particular—should prioritize:
- Wearing appropriate protective gear when handling potential contaminants in the workplace or home projects.
- Regularly testing drinking water for lead or arsenic, especially in older homes.
- Limiting consumption of high-mercury fish such as shark, king mackerel, and tilefish.
- Exercising caution with herbal remedies of uncertain provenance or those not regulated by reputable authorities.
Community involvement and advocacy can also make a meaningful difference. Demanding stricter regulations, reporting environmental spills, and supporting local remediation efforts create safer living conditions.
Recent Advances in Treatment
Research and innovation are continually evolving the landscape of heavy metal detoxification. Among the most promising developments is the introduction of oral agents like HOPO 14-1, designed to selectively bind and remove radioactive and toxic metals with minimal side effects. This treatment, still under investigation, holds significant promise for future management strategies, especially in populations exposed to environmental disasters or industrial accidents. Additionally, precision diagnostics and wearable monitoring technologies offer real-time assessment of internal toxin burdens and individualized treatment adjustments, underscoring the future direction of more proactive, person-centered care.
Conclusion
Heavy metal toxicity remains a significant modern health hazard, but increased awareness, reliable screening, and science-driven therapies now offer meaningful hope. By adopting practical preventive measures, recognizing early warning signs, and seeking out evidence-based heavy metal toxicity treatment from qualified professionals, individuals can dramatically reduce their risks and safeguard long-term health. Remaining informed and attentive is the most powerful tool available in the fight against these invisible toxins.